Hey there! This post may contain affiliate links. As an Amazon Associate, I earn a teensy commission from qualifying purchases when you buy through these links (at no additional cost to you). For more info, please check the full disclaimer.
Epidural injections are usually administered in childbirth and surgical procedures to reduce the sensation of pain. While they are considered relatively safe, mild adverse effects may appear after using an epidural in pregnancy.
In rare cases, severe symptoms in mothers or infants have also been observed.
Per a research, approximately six million women in the United States give birth every year, out of which 1.4 million prefer epidurals to relieve pain during labor.
This blog will explore the side effects of administering an epidural for labor.
What are Epidural Injections?
An epidural is a pain relief method that inhibits nerve transmission in the abdominal and pelvic regions.
Epidural injections involve a procedure in which local anesthesia is injected into the space surrounding the spinal cord.
Epidural injections are named after the site of medicine administration called epidural space – the area between the dural membrane and the spinal cord.
Administrating the epidural injection in this spot can block the nerve impulse, preventing the brain from registering the pain. However, they do not cause loss of consciousness or loss of movement in the lower parts of the body.
Epidural in pregnancy involves a small tube called a catheter attached to the mother’s lower back. The anesthesiologist can easily inject the anesthesia through the catheter whenever required. The epidural usually takes 10-30 minutes to relieve pain.
Read More: How to Enjoy First Trimester of Pregnancy
How Do Epidural Injections Work?
Epidurals in pregnancy involve the administration of local anesthesia, which causes numbness in the lower back and pelvic region. Some concentrations of opioid medications are also added in epidural injections to offer enhanced pain relief.
Local anesthesia in epidurals works by inhibiting the transmission of nerve impulses from the spinal cord to the brain so that the patient feels less pain.
The exact mechanism of epidural in pregnancy depends on the type administered. The two major types of epidural are:
- Standard Epidural
Standard epidural uses the catheter placed in the mother’s spine to administer local anesthesia, such as bupivacaine, lidocaine, chloroprocaine, and opioid medicine like fentanyl and sufentanil.
As these medications start to show their effect, the mother will gradually lose feelings in their legs, making it challenging for her to move without assistance.
- Walking Epidural
A walking epidural during pregnancy involves a mixture of epinephrine, anesthesia, and opioid medications in lower concentration than the standard epidural.
Due to the smaller dosages, the mother will have sensations in her legs, allowing her to support her weight and move around without requiring assistance.
According to research published in The Lancet, women who opted for a walking epidural for pregnancy were more satisfied with analgesia, and fewer women complained of leg weakness at the end of labor.
Read More: How to Enjoy Second Trimester of Pregnancy
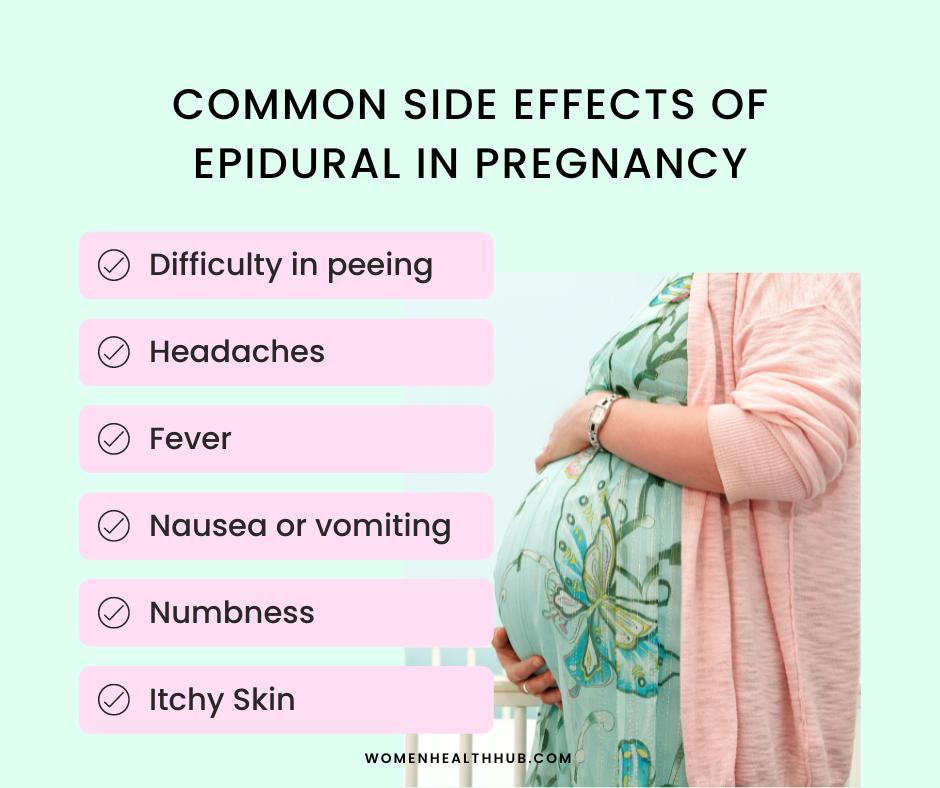
What are Some Common Side Effects of Epidural In Pregnancy?
Many women feel unwanted side effects after administering an epidural during pregnancy. These effects differ from patient to patient and are mostly based on the type of medication used. Your anesthesiologist may change the drug if you consult them regarding the severity of your symptoms.
Let’s discuss some of the side effects commonly seen with the use of epidural in pregnancy:
1. Low Blood Pressure
Epidurals block the transmission of nerves, preventing the blood vessels from contracting, which decreases the overall blood pressure. Due to low blood pressure, many mothers experience light-headedness and dizziness.
About 14% of women who uses epidurals for pregnancy experience a drop in blood pressure. Low blood pressure also affects the blood supply to the placenta, putting the baby at risk. Intravenous fluid (IV) is given to reduce the risk of blood pressure falling too low.
2. Difficulty Urinating
About 15% of women complain of urinary retention after receiving an epidural during labor. The epidural paralyzes the nerves surrounding the urinary bladder, making it difficult for the mothers to urinate.
Many women have trouble urinating, feel like their bladder is not entirely empty, or can only pass small amounts of urine.
A catheter is usually placed that collects urine in a separate bag. You should regain bladder control as the effects of the epidural start to subside.
Read More: 7 Critical Signs of Gestational Diabetes
3. Itchy Skin
Epidural medications, mainly opioids used in pregnancy, can cause itchy skin in women. According to a study conducted in 2021, greater doses and concentrations of morphine in epidural increase the incidence of pruritis.
If itching persists, your doctor may change the medication used with the epidural in pregnancy to alleviate the adverse effects.
4. Fever
Fever has been observed in about 23% of women that use an epidural during pregnancy. While the exact mechanism is unknown, many studies have suggested that epidurals induce inflammation and alter the body’s thermoregulation system, resulting in higher body temperature.
5. Nausea and Vomiting
Opioid painkillers, including epidurals, can sometimes cause nausea and vomiting. The reason behind this is unknown, but a study has observed that 2.4% of women taking walking epidurals complain of nausea, and 3.2% have vomiting. In comparison, this percentage was lower in women who preferred standard epidurals.
Read More: 25 Best Foods to Relieve Heartburn in Pregnancy
6. Back Pain
Many women experience soreness in the area after inserting an epidural in pregnancy. The back soreness caused by epidurals is temporary and should subside within a few days.
In many instances, back pain is due to the added weight of the baby during pregnancy and may not necessarily be due to epidurals.
7. Numbness After Birth
After birth, many mothers report numb legs and feet. As the effect of epidural starts to wear off, most women can wiggle their toes and move their legs. The numbness lasts about two hours but usually depends on the type of epidural given.
8. Tremors
Tremors are a common neurological side effect of epidural in pregnancy. Tremors are seen in 18% of women thirty minutes before delivery. Shivering-like tremors are not associated with thermoregulation as mothers have average body temperature and do not complain of coldness. However, wrapping a warm blanket around these mothers sometimes helps with shivering.
Read More: 18 Best Home Remedies for Easing Pregnancy Acidity
What are Some Rare Effects of an Epidural in Pregnancy?
At times, epidural during pregnancy may also show rare and unprecedented side effects in only a handful of mothers.
Let’s discuss some unusual side effects that some women have reported.
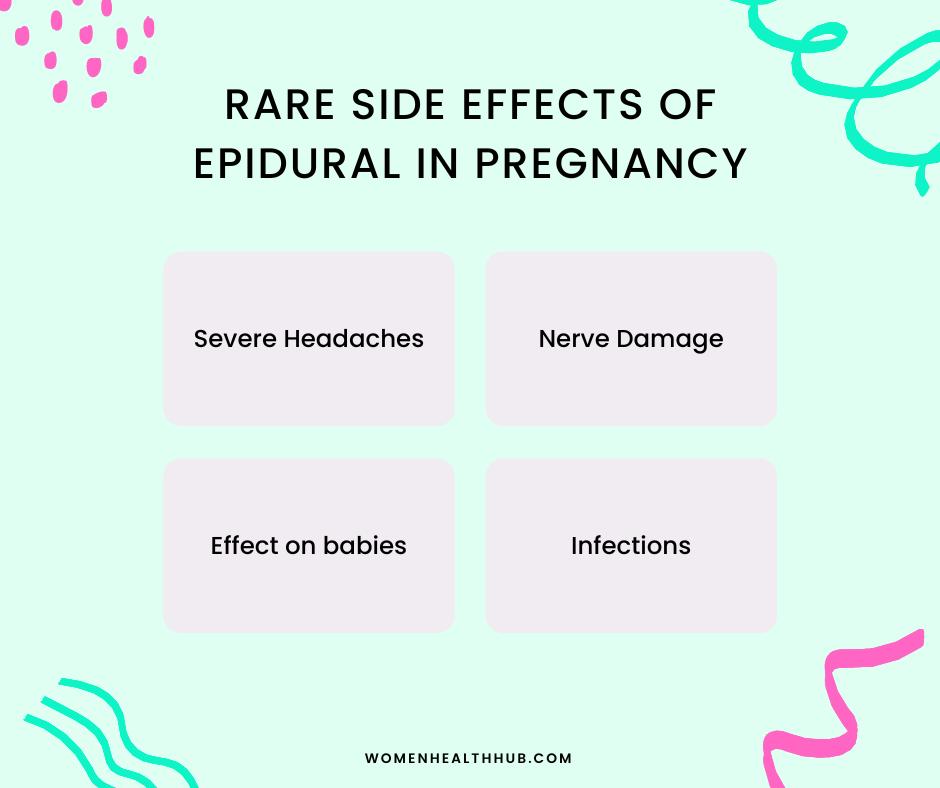
9. Severe Headaches
Sometimes when injecting the epidural for pregnancy pain, the needles may be inserted too deep into the dural space, causing a dural puncture. The spinal fluid leaks out of the dural puncture causing severe headaches and drowsiness in mothers.
Dural punctures are quite rare, occurring in 1% of all mothers receiving epidurals.
Read More: 9 Best Pregnancy Yeast Infection Treatments
10. Nerve Damage
Nerve damage is a rare complication of epidural in pregnancy. It usually causes temporary damage to a single nerve or a group of nerves in the lower body. Accidentally hitting a nerve when injecting an epidural, blood clots near nerves, or inadequate blood supply due to hypotension can lead to nerve damage.
Only 1% of women who give birth with epidurals complain of leg weakness, numbness, or pain in the lower extremities due to compression of nerves in labor.
11. Infections
Before injecting the epidural during pregnancy, the skin is cleaned with anti-septics, and a sterilized needle is used. Sometimes women may get infections at the site of epidural administration, causing a mild bacterial infection or formation of an epidural abscess.
Very rarely, some women may develop severe infections such as osteomyelitis or meningitis.
Read More: 19 Serious Pregnancy Infections + Tips to Avoid Them
12. Effect on Baby
Like other substances, epidural in pregnancy can also pass through the placenta and enter the baby’s bloodstream. These medications can lower the respiration rate of babies before birth.
In 2014, research showed that respiratory distress is more likely to occur in neonates due to epidural use in pregnancy.
If an epidural cause low blood pressure in mothers, it can also affect the baby’s heart rate, putting the baby’s life at risk.
According to a study published in 2021, the use of epidurals during pregnancy increases the risk of neonatal infection, including sepsis, pneumonia, and undefined infections in babies.
Read More: 11 Tips to Prevent Birth Injuries
Does the Use of Epidural Lead to Assisted Births?
About two-thirds of women, when giving birth, opt for epidural in pregnancy. Research published in 2005 showed that using epidurals reduces the cervix’s dilation rate, which slows labor’s progression into the active phase.
Contrary to popular belief, mothers can still feel contractions and push the baby out. However, many women may need assistance, like using a vacuum or forceps during vaginal delivery.

According to a study published in 2015, epidural increases the risk of instrumental delivery but was not associated with the Ceasrian section.
Another research published in 2019 concluded that using epidural analgesia in pregnancy could lead to instrumental delivery, C-section, and even abnormal fetal head position.
The Bottomline
Epidural in pregnancy is the most effective method for pain relief. However, it may be accompanied by a series of potential side effects. From headaches, hypotension, and skin problems, to infections and nerve damage, many hazards exist before opting for epidurals.
It is also important to note that all women do not experience negative consequences, nor will they have the same side effects. Remember, no two birthing experiences are the same. Consider your own needs and preferences as you prepare for your labor.
References:
- https://pubmed.ncbi.nlm.nih.gov/16008883/
- https://pubmed.ncbi.nlm.nih.gov/24170528/
- https://clinicaltrials.gov/ct2/show/NCT02149680
- https://tinyurl.com/bmc-pregnancy
- https://tinyurl.com/headache-epidural








